Hemodialysis Access Care
What is Hemodialysis?
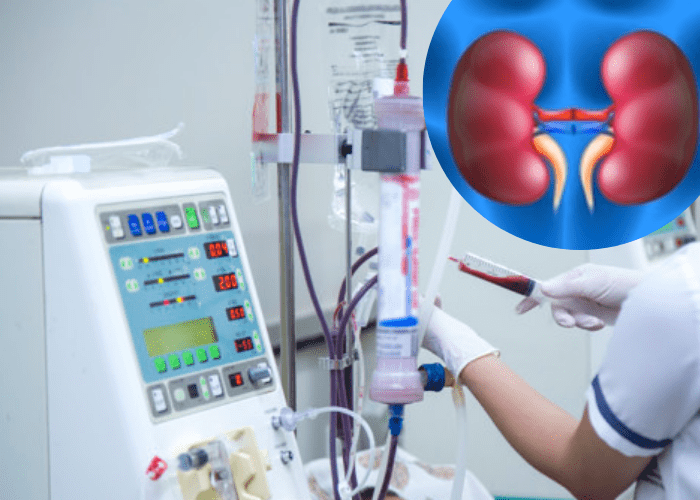
In medicine, dialysis is the process for patients who experience kidney failure. During such failure, the kidney fails to cleanse the blood of wastes, including urea or any extra fluid. Hemodialysis, also called dialysis, is used to withdraw blood from the body into a machine. This procedure uses a special membrane (Dialyzer) to filter wastes and extracts excess fluid from the blood. It also restores the electrolyte balance in the blood. Dialysis usually takes about three hours and occurs thrice a week. Avail the best Hemodialysis Access Care in Mumbai with us.
What is Hemodialysis Access?
Hemodialysis Access – also called “Vascular Access” – is a way to withdraw blood for hemodialysis. Due to the need to withdraw faulty blood from the body and replace it, a means for accessing the patient’s blood circulation through hemodialysis becomes necessary. There are three different types of procedures for this, some of which are used interchangeably: Dialysis Fistula, Graft and Catheter. All of these techniques can remove and supply large amounts of blood into the body at the same time–about one quart per minute.
